Back Pain Untangled

John is a 45 year young gentleman. He has served many years as a firefighter saving lives. He had an episode of severe back pain in his 20s while playing lacrosse. That injury made him bedridden for few days. He saw a chiropractor back then and was up and running in no time. His job and two kids keep him running day in and day out.
In June 2020, John was lifting a heavy piece of furniture with his friend when he felt a small “pop” in his lower back. He did not think much about the incident. He woke up with severe back stiffness the next morning. Covid pandemic related restrictions were still ongoing. He avoided going to his family doctor. His old chiropractor was not seeing patients either. He iced his back for few days, but his spasms just would not resolve. After one week of suffering, he ended up at an urgent care facility. He saw by a doctor briefly. X-ray done on site were “normal”. He was given a prescription-grade-ibuprofen along with a muscle relaxer and reassured that he would be better soon.
Before we begin John’s story further, let’s learn few things about spine pain.
Little Introduction
Spine Pain (Neck, Mid or Low-Back) requires little (to no) introduction. It is the leading cause of disability worldwide. There is ample of literature published on this topic. A simple google search can lead you to an exhaustive material to review for weeks, if not months. If you are interested in knowing facts, numbers or statistics, I urge you to look at John Elflein’s report for more details.
To impress you with numbers, consider these three:
39%
PERCENTAGE OF US ADULTS WHO EXPERIENCED BACK PAIN IN LAST 3 MONTHS
54%
PERCENTAGE OF US ADULTS WHO HAD NECK OR BACK PAIN FOR 5 YEARS OR LONGER
73%
PERCENTAGE OF US ADULTS WHO TOOK NON-STEROIDAL ANTI-INFLAMMATORY DRUGS LIKE IBUPROFEN FOR NECK OR BACK PAIN
The purpose of this article is not to exhaust you further about the growing issue, but we are here to understand how medical providers approach the topic. I will be using the term “back pain” throughout this article, since low back pain is more common than neck pain, but similar fundamentals are applicable to both problems.
Know The Basics
Back pain affects people of all ages. It takes toll on their personal lives and remains a leading cause of economic loss at work place. Before you start to learn about how doctors approach your back pain, I would suggest knowing about the spine itself. This will help in understanding the upcoming sections.
As the video outlined, spine is a complex structure of interconnecting bones, ligaments, muscles, joints and cartilage; all working together to provide support, strength, and flexibility. It sheathes spinal cord and nerve fibers, which work as a cable connecting your body to brain. This complex structure leaves the spine susceptible to injury and pain. Pain could originate from one or more of these structures, presenting remarkably similar in many settings. Back pain is thus a puzzle to solve from get go.
What’s Your Problem?
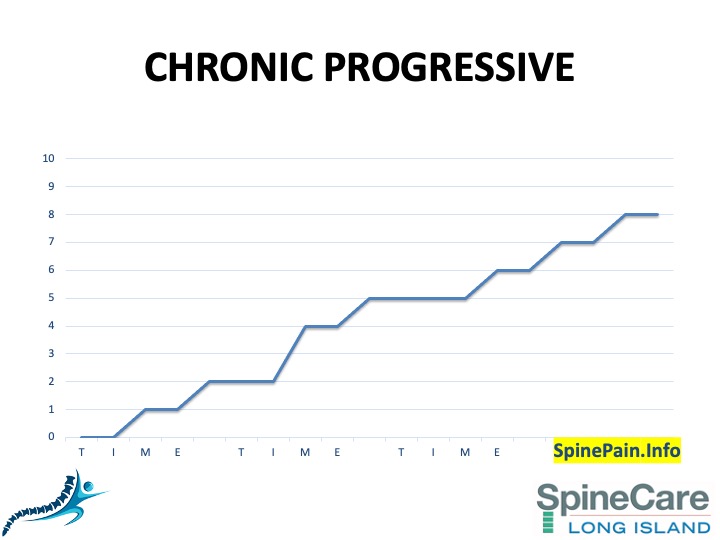
Many doctors are not passionate in solving the back pain riddle. There is a general belief among physicians that over 90% of acute back pain patients get better over time (with or without aggressive treatment options). They tend to ignore symproms early on based on this notion. This conviction stems from an old scientific study. Researchers have recently looked closely into the natural progression of back pain. They concluded that back pain is not a self-limiting problem, but rather a recurrent and sometimes persistent disorder.[1], [2], [3], [4], [5], [6] New knowledge indicates that most low back pain episodes are short lived, at least in the primary care setting. Nevertheless, in the long term, low back pain often runs a persistent course with around two-thirds of patients estimated to be in pain after 12 months. Some individuals never have low back pain, but most have it on and off or persistently. When doctors first see a patient with new onset of back pain, it is hard to predict the trajectory their symptoms could take.
Understanding back pain becomes more complex when you are informed that many people with actual structural problems on their spine (disc bulges, disc herniation or tears, spinal arthritis, minor fractures, benign tumors etc.) may not ever feel back pain. Thus, diagnosing a cause of back pain is not easy. It requires attention to small details, a thorough examination, as well as ordering and analyzing specific tests (X-Rays/CT scan/MRI) for a given person. It may require treatment trials, like core strengthening by a physical therapist, or traction by a chiropractor. It may involve trial of oral medications like anti-inflammatories or muscle relaxers or delivery of Novocain or cortisone like medications at certain parts of your spine (spinal injections). Outcomes from each of these steps add information that eventually helps doctors reach a specific diagnosis.
Where To Start?
By the time you are reading this article, you our your suffering loved one might have seen a handful of doctors. It is expected that you have spoken to your primary doctor, or been to an urgent care facility or emergency department. Don’t feel discouraged if you were not taken “seriously”. As I had outlined earlier, since many people do improve after the initial severe episode, it is natural for physicians to “downplay” your first episode of neck or back pain. Now that your initial episode has not resolved, or grown into a bigger/persistent issue, it is time to take your pain more seriously and seek help from a spine specialist.
Spine or back pain specialists come from several diverse medical streams and look at spinal problems differently. A physical therapist’s or an acupuncturist’s approach is distinct from a chiropractor’s way of handling back pain. A spine interventionalist has a different objective than your spine surgeon. It is important to get opinions from more than one expert and educate yourself as much as possible.
At SpineCare, we work closely with your physical therapist or your chiropractor to help us formulate a minimally invasive and tailored treatment plan. Our pain doctors and spine surgeons work together understanding each individual case guiding us to our core principle of superior patient outcomes.
Approach to Spine Pain
Now that you have learnt the basics of spine structure, and the important issues that doctors face, you are ready to learn the simple approach to spine pain. There are few important questions to address:
- Is you ongoing spine pain recent, a pattern of episodic pain, or a chronic progressively declining condition? (Apples & Oranges)
- Do your symptoms match up to the structural changes seen on the MRI? (Pieces of Puzzle)
- Is your pain axial, radicular, or mixed? (The Big Three)
- Is there a need to implement spine diagnostics to identify the source of your pain? (The Culprit)
- Do you have any concerning red flags to warrant further testing or involvement of additional specialists?
- Red Flags for Back Pain
- History (things your doctor would ask during discussion)
- Cancer
- Unexplained weight loss
- Immunosuppression
- Prolonged use of steroids
- Intravenous drug use
- Urinary tract infection
- Pain that is increased or unrelieved by rest
- Fever
- Significant trauma related to age (e.g., fall from a height or motor vehicle accident in a young patient, minor fall or heavy lifting in a potentially osteoporotic or older patient or a person with possible osteoporosis)
- Bladder or bowel incontinence
- Urinary retention (with overflow incontinence)
- Physical Signs (things your doctor might see on examination)
- Fever
- Saddle anesthesia
- Loss of anal sphincter tone
- Major motor weakness in lower extremities
- Vertebral tenderness
- Limited spinal range of motion
- Neurologic findings persisting beyond one month
- History (things your doctor would ask during discussion)
- Red Flags for Back Pain
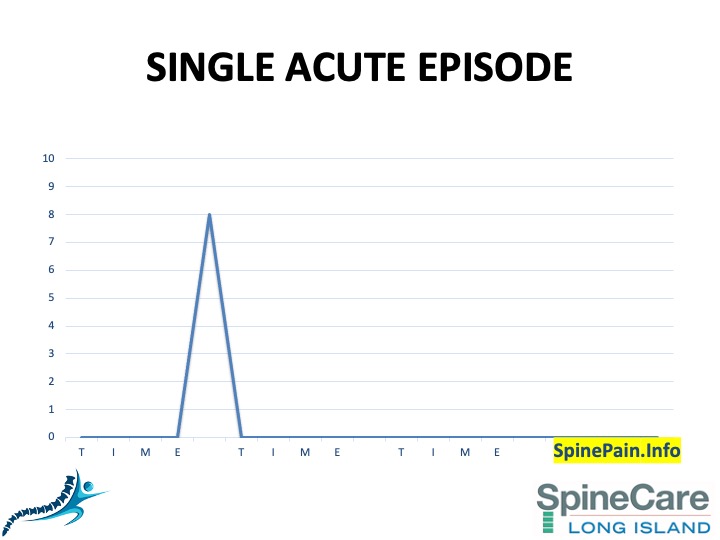
Apples & Oranges
After red-flags have been ruled out, the first thing most spine specialists look for is the onset and pattern of your neck or back pain. It is important to know whether your ongoing spine pain is acute (recent), a pattern of episodic pain, or a chronic progressively declining condition. The difference is important. No two back pain patients are same, and no two episodes in the same person could be assumed to be similar. You may have fallen off a skateboard or hurt yourself while playing sports as a teenager that caused the initial episode of back pain in your life, but if you lifted a heavy piece of furniture a decade later, it is (probably) not the same pain you suffered decades ago. Although “acute” episodes could be the start of a problem which may eventually grow into an episodic persistent pain or a chronic relentless problem, it is investigated and treated differently.
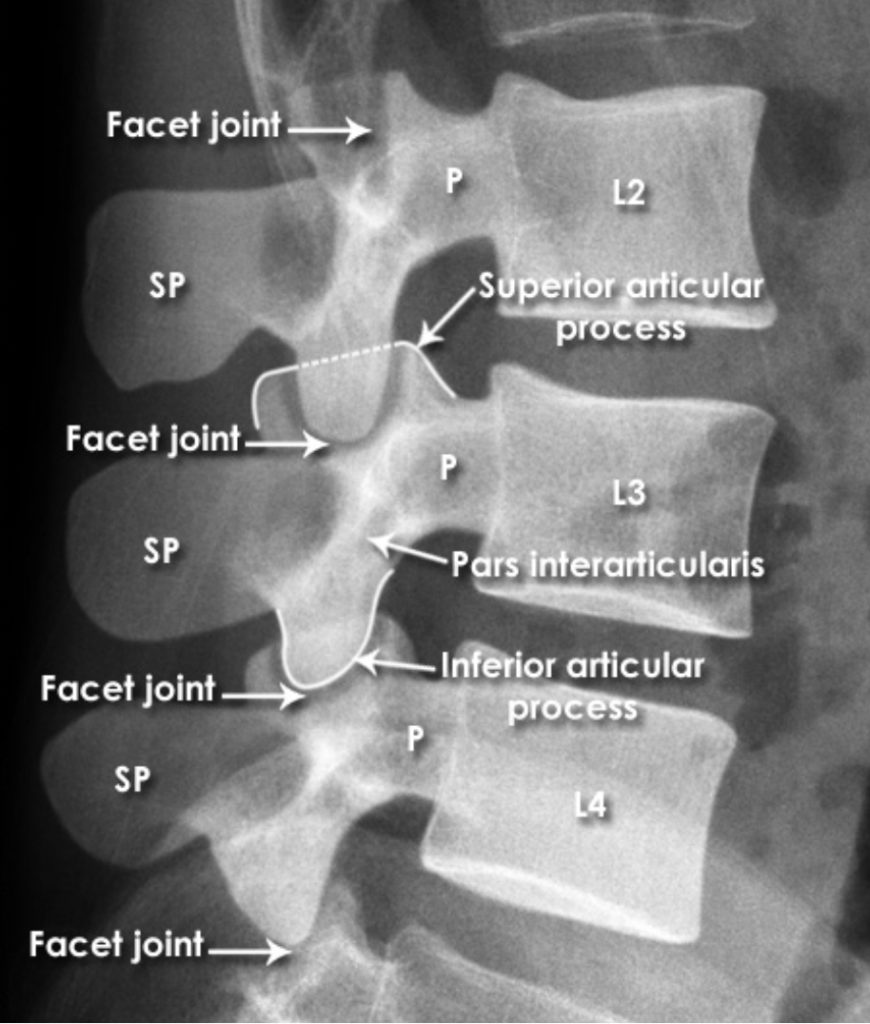
Frequently, we see teenagers coming to our offices with neck or back pain related to muscle sprains, minor injuries to spinal ligaments or facet joints, and at times benign fractures (spondylolysis). We also see many younger people injured from traffic accidents or work place falls leading to soft tissue injuries, minor disc tears (annular fissures), disc herniations, or facet joint injuries. Lastly, we see people in golden yeas suffering from degenerative conditions like osteoporosis related compression fractures, arthritis of spinal facet joints, degenerative disc disease or spinal stenosis. Age is not the clear criteria for these conditions, but simply an indicator. We see ample of younger people with degenerative conditions and senior citizens with sprains or minor disc issues.
Pieces of Puzzle
Based on the initial assessment of your episode, your doctor may decide to order X-Rays, CT or MRI scan to assess your condition further. Each of these tests provide different information. Before we go further, let’s discuss few related topics.
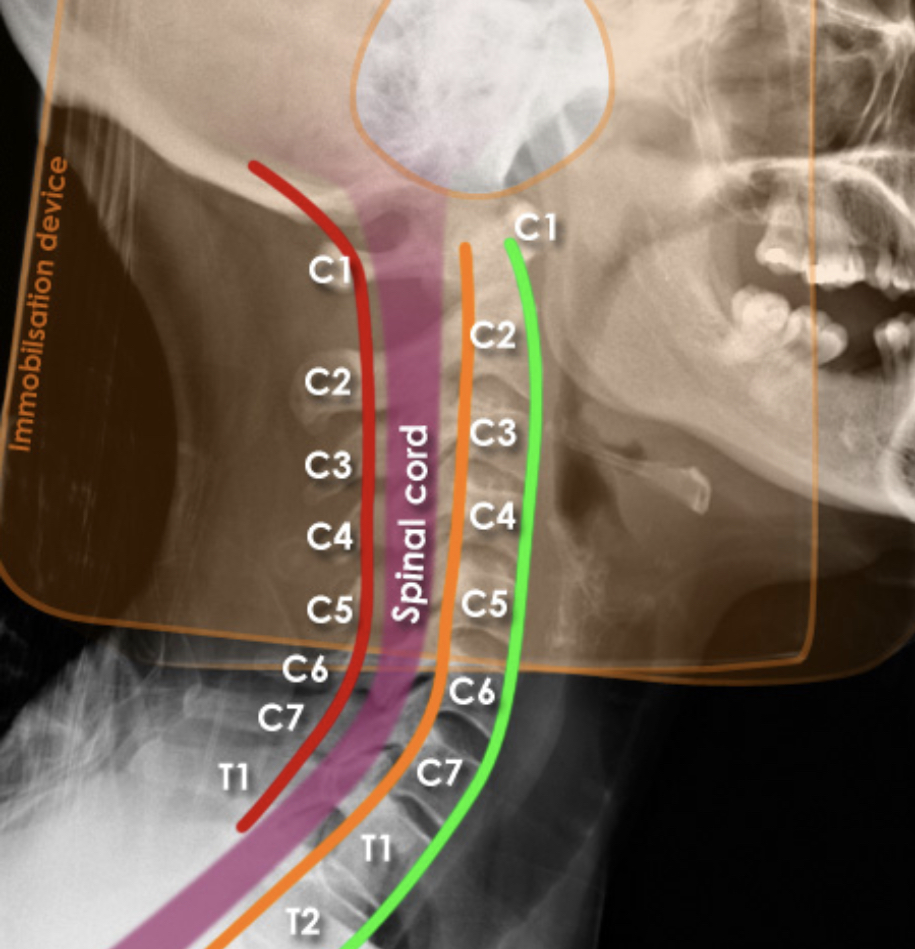
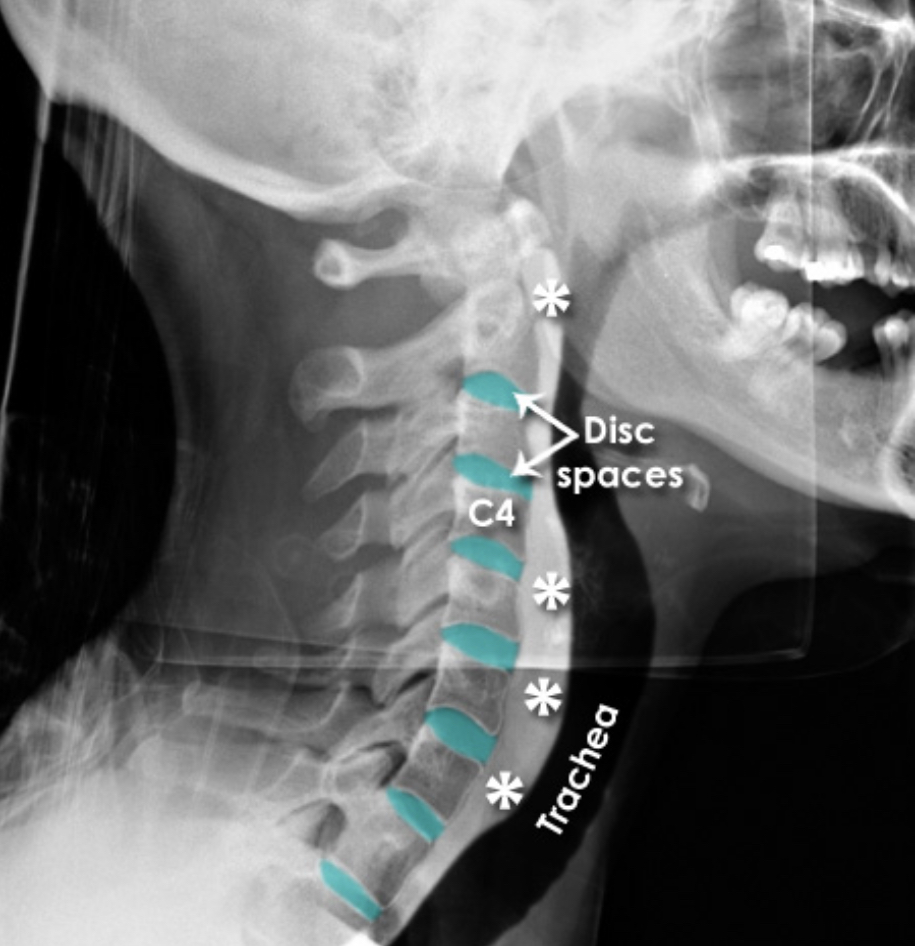
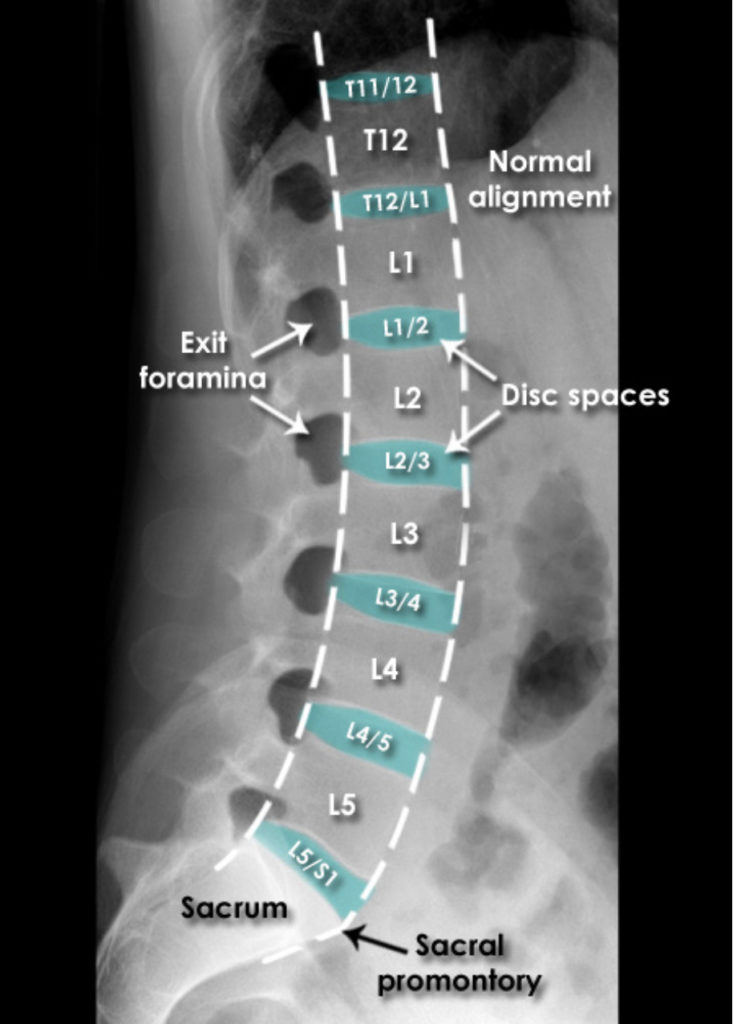
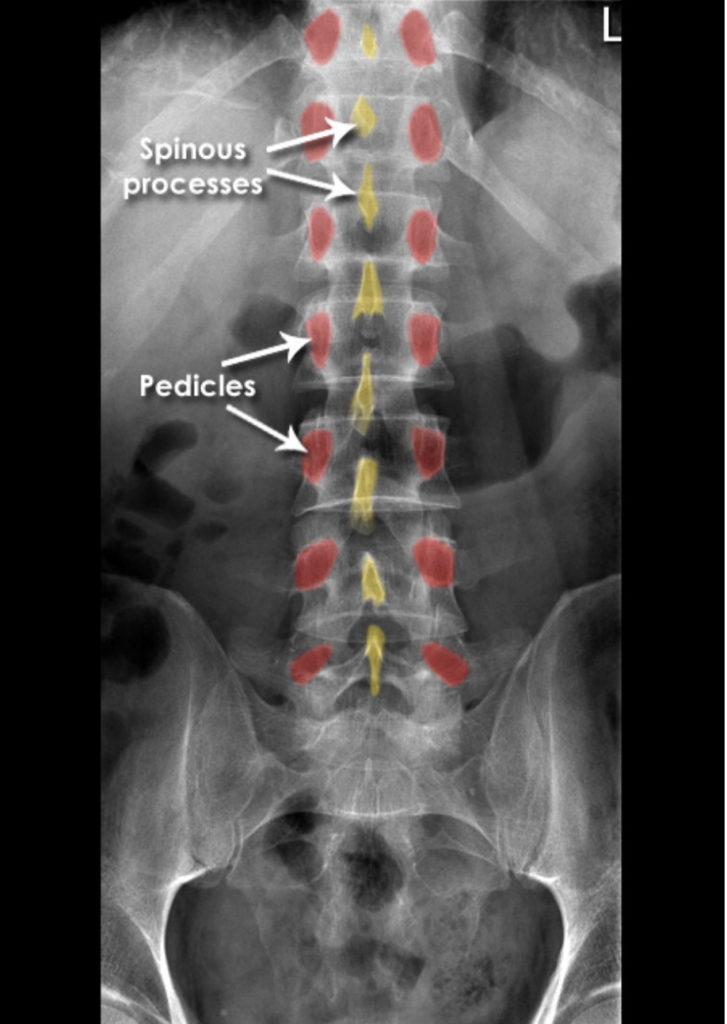
X-Rays [7]
X-rays (radiographs) are the most common and widely available diagnostic imaging technique. They take seconds to be completed. They frequently do not require any insurance authorization. They (mostly) show bony structures and provide information about alignment and health of your spinal bones. They help to rule our any major fractures. Although we cannot see any soft tissue structures (muscles, ligaments, discs, nerves) on X-rays, few details on them could be suspected. For instance, if the distance between the two spinal bones is narrowed, it suggests underlying degenerated or herniated disc. If the adjacent bones next to a narrow disc space show signs of degeneration, it is more likely a degenerative disc condition.
Patients routinely ask us if the test would be harmful to their body. I am going to briefly outline the possible radiation risk related to each test. Sievert (Sv) and millisievert (mSv) are metrics or units most commonly used to quantify the biological effect of radiation on human body. Taking these into account, millisieverts describe what’s called the “equivalent dose.” A lumbar spine X-ray exposes you to 1.5 mSv dose.
CT Scan (Computer Tomography)
Computed tomography (CT) is an imaging tool that combines x-rays with computer technology to produce a more detailed, cross-sectional image of your body. A CT scan is way more sophisticated than X-rays. They require 5-10 minutes to complete and exposes you to a lot more harmful radiation than an X-ray. Typically, lumbar spine CT scan exposes you to 6 mSv of radiation dose.
In a 2009 study from Brigham and Women’s Hospital in Boston, researchers estimated the potential risk of cancer from CT scans in 31,462 patients over 22 years. For the group as a whole, the increase in risk was slight — 0.7% above the overall lifetime risk of cancer in the United States, which is 42%. But for patients who had multiple CT scans, the increase in risk was higher, ranging from 2.7% to 12%. (In this group, 33% had received more than five CT scans; 5%, more than 22 scans; and 1%, more than 38). One CT scan, thus, is unlikely to cause any relevant hard to your body.
CT scans give us a lot more details on bony structures of spine, but still provide less than optimum information on soft tissues. It requires an insurance authorization. If you happen to have an implanted metal device in your body, CT might be the only option for you. MRI is frequently contraindicated in these situations. Consult our office for details regarding your specific situation.
MRI Scan (Magnetic Resonance Imaging)
Magnetic resonance imaging (MRI) is another diagnostic imaging technique that produces cross-sectional images of your spine. Unlike CT scans, MRI works without harmful radiation. It uses magnetic fields and a sophisticated computer to take high-resolution pictures of your bones and soft tissues. You may not be able to get MRI scan if you have a pacemaker, implants, metal clips, or other metal objects in your body.
MRI is a gold standard test for spine. It does not show exceptional details on spinal bones, but provides a lot more information on soft tissues (spinal ligaments, discs, spinal cord and nerves). MRI frequently requires an insurance authorization process and our office can help you through this process.
Once these scans are available, a spine specialist is ready to put the pieces of information together to form an initial diagnosis and identify the source of your problem. This part is challenging, but important. Almost a third of normal healthy people, who are not complaining of any spine pain, happen to have a degenerated or herniated disc, or other positive findings on their CT or MRI scans. Our goal is to match your reported pain, physical examination and MRI findings together. If the three match up well, count your blessings since your case would not be disputed between experts. You can expect consistent recommendations from different spine experts.
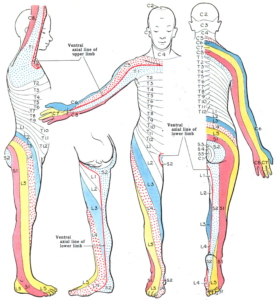
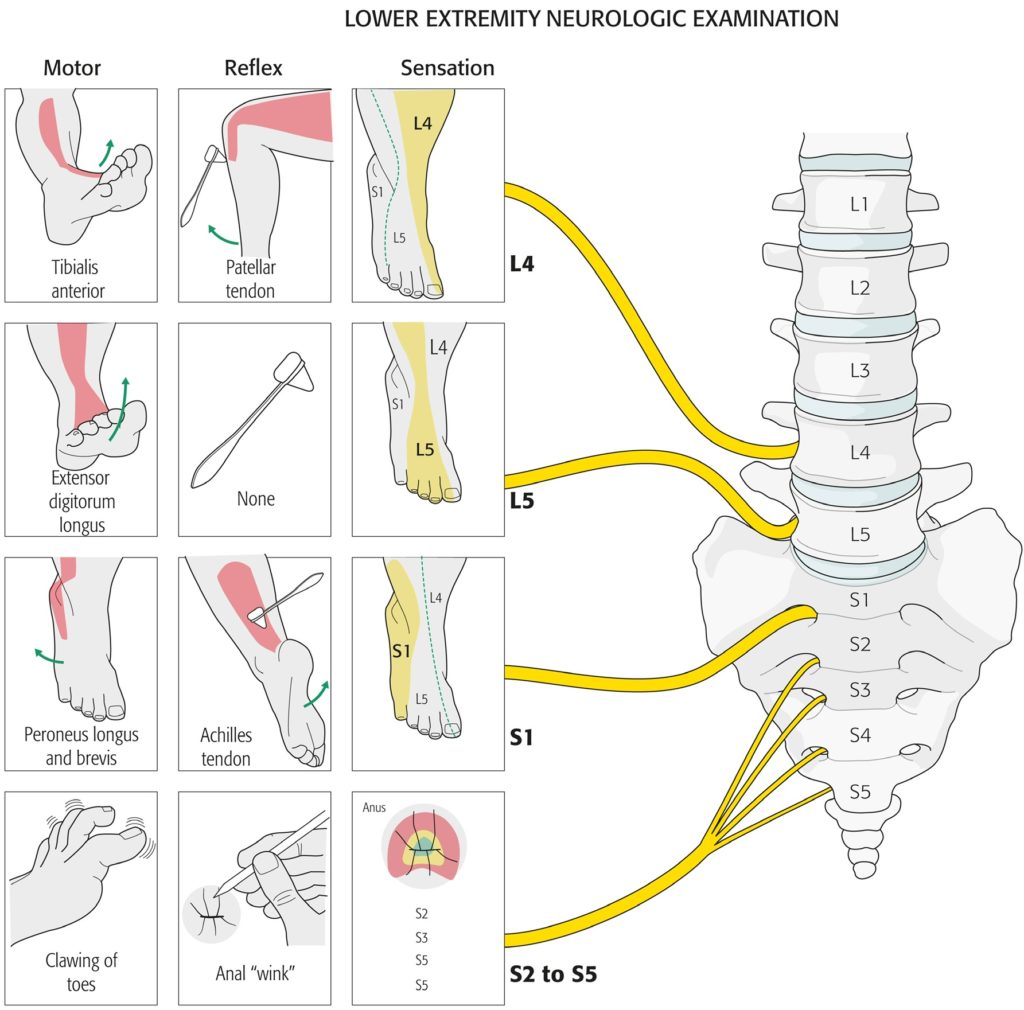
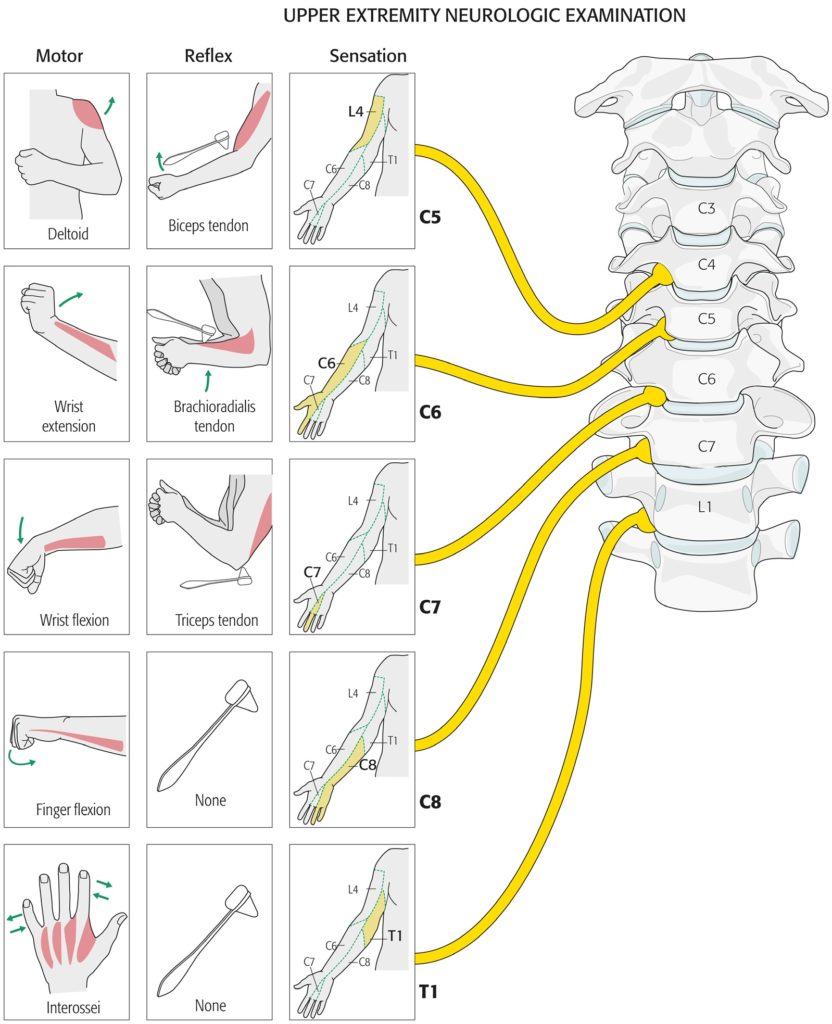
Let us discuss a more specific case. If you are having pain which radiates from lower back into the outer part of your thigh (between hip and knee), crossing below the knee to outer part of your lower leg (knee to ankle) and travels to the top of your foot and big toe; is is called as “radicular pain in L5 distribution”; the area supplied by L5 nerve root (shaded yellow in the dermatome map as depicted). The muscle likely to be weak, when L5 nerve root is pinched, is extensor hallucis longus (EHL). This muscle helps in elevation of your big toe. The reflex likely to be blunted is achilles tendon reflex (checked by your doctor striking your achilles tendon with a refill hammer). When all of these 3 are present, and your MRI shows a disc herniation compressing the same nerve root, it confirms a diagnosis of L5 radiculopathy. We will use this information with one of our cases soon.
I must emphasize that it is not common for us to come across simpler cases like the one we discussed. For reference, here are the dermatomes (area of skin supplied by a single nerve root), myotomes (group of muscles supplied by one nerve root) and corresponding reflex changes are outlined below.
One of the frequent challenge we face everyday in the spine world is the lack of consistent findings in most cases to reach a conclusive diagnosis. A person who has a clear history of a “pinched left L3 nerve” may not show a consistent neurological findings (numbness or weakness in a different nerve distribution). At times when these two do correlate, MRI may show a disc herniation on the opposite side or at an unexpected spinal level. Solving these cases everyday is what makes our job interesting.
We prefer to give ample time to our patients to speak about their pain or other symptoms. We like to examine patients ourselves. We love to see the MRI films personally, and not depend on a report read by another doctor sitting in a dark room. We consider these pieces of information vital to solve the underlying problem. We are fascinated with every single spine pain case. Our learning about the complexities of human spine never stops. When necessary, we involve more minds to your case during the same visit. It is not uncommon for one of my SpineCare colleagues to walk into my office, present a case like a medical student, show me the films related to the case and ask for my opinion. I have no shame in doing the same when your problem is perplexing to me.
The Big Three
AXIAL PAIN
- Pain mostly around the core: Neck, mid-back or low back
- Pain may radiate to shoulder (from neck), flank (from mid-back) or buttocks/hips (from low back)
- Some of the common causes of this type of pain is degenerative disc disease, modic changes affecting vertebral end plates, annular tears, injury or arthritis of facet joints, sacroiliac joint issues, or muscle sprains.
RADICLULAR PAIN
- Pain predominantly radiating down arm, chest wall to belly/groin, or mostly traveling down the leg
- Some of the common causes of radicular pain is herniated discs, foraminal or central spinal stenosis or piriformis syndrome.
MIXED PAIN
- Pain affecting both core and has a radicular or non-radicular component
- Most common variety off the three
- Common causes include a long list of spine condition outlined below.
The Culprit
Once we have gathered the pieces of puzzle, we tend to formulate a preliminary diagnosis; the cause of spine pain or the real culprit. On most occasions, the diagnosis can be made based on the description of pain, physical examination findings and MRI results. At times these pieces do not add up clearly. In those handful of situations, spine diagnostics come handy. Spine Diagnostics is an area of interventional pain medicine where a small doses of Novocaine-steroid mixture is injected at designated targets to confirm a diagnosis. Although these test injections carry a risks of false positive or negative responses, but overall, along with the MRI findings, they add to the accuracy of diagnosis. These diagnostic injections must be performed in a controlled fashion by a trained and experienced professional. Another spine diagnostic modality is EMG and nerve conduction study. This test is performed by an experienced neurologist.
CASES
Now that we have covered few basics, let’s discuss few cases. We left John’s story in the middle. Let us catch up on his progress.

Last we discussed, John had hurt his back while lifting a heavy piece of furniture with his friend. He went to an urgent care facility. He was given ibuprofen along with a muscle relaxer and reassured that his pain would soon resolve. Unfortunately, John’s misery did not end there. He went back to the urgent care center 4 days later. Now his back pain had started radiating into his left leg (buttock, outside of his left thigh, down the calf to the top of his left foot). During this visit, the doctor told him that he had “sciatica”. John was given a steroid pack and referred to a physical therapy center. Within two days of taking steroid pack, his back and leg felt better. He managed to find a physical therapy center near his home. They had just started accepting new patients. John started with PT sessions, but unfortunately within a week his back pain returned with a vengeance. His sciatica was worse and now his left leg felt numb. John was getting scared of losing his livelihood, or worse; getting paralyzed. He called his family doctor and was urgently referred to our center.
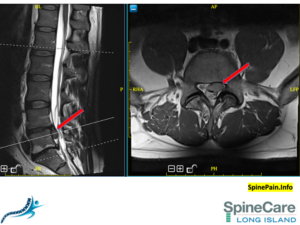 John visited at our office in late July. We ruled out the concerning “red-flags” first. On examination, we noticed numbness in his left L5 dermatome (Look at the dermatome chart shown earlier. L5 dermatome is highlighted in yellow color). John’s leg muscles strength was normal. He did favor his left leg due to pain, but he was able to walk with discomfort. We sent John for MRI the same day. We saw him back at the office the next morning. This is the picture of his lower back MRI. The red arrows point a large size “extruded disc herniation” on the left side. A formal diagnosis of lumbar radiculopathy from a herniated disc was made.
John visited at our office in late July. We ruled out the concerning “red-flags” first. On examination, we noticed numbness in his left L5 dermatome (Look at the dermatome chart shown earlier. L5 dermatome is highlighted in yellow color). John’s leg muscles strength was normal. He did favor his left leg due to pain, but he was able to walk with discomfort. We sent John for MRI the same day. We saw him back at the office the next morning. This is the picture of his lower back MRI. The red arrows point a large size “extruded disc herniation” on the left side. A formal diagnosis of lumbar radiculopathy from a herniated disc was made.
John met two team members the same day during his visit to our office. Our spine surgeon recommended maximizing conservative modalities, with a cautious approach. He was advised to check for any leg weakness on a daily basis using a home based tests. He underwent a selective nerve root block and became pain free in a week. He was sent back to physical therapy for ‘core strengthening’, to avoid any future issues. At 3 months, John feels back to his normal self. Since clinical recovery precedes radiological recovery, no follow MRI was considered necessary.
Keep following this article. We will discuss more interesting cases in the coming weeks.
We Are Not Done
I am trying to update this article as much as time permits me. I will continue to write more in coming weeks. Please read about individual spine pain conditions in the next sections.
Spine Conditions
Spinal Column Conditions
-
- Spondylolisthesis and Spinal Instability
- Spinal Stenosis: Central and Foraminal
- Coccydynia
- Skeletal irregularities
- Scoliosis (a curvature of the spine)
- Lordosis (an abnormally exaggerated arch in the lower back)
- Kyphosis (excessive outward arch of the spine)
- Miscellaneous congenital anomalies of the spine
Spine Bone/Joints Conditions
-
- Vertebrogenic Pain
- Compression Fracture
- Spondylolysis
- Facet Syndrome: Sprain, Fracture, Arthritis
- Spina Bifida: Involves the incomplete development of the spinal cord and/or its protective covering and can cause problems involving malformation of vertebrae and abnormal sensations and even paralysis
- Osteoporosis: A progressive decrease in bone density and strength that can lead to painful fractures of the vertebrae
- Vertebral Osteomylitis
Disc Conditions
Spinal Nerve Conditions
Conditions Mimicking Spine Diseases
Post-Surgical Conditions
Non-spine sources
-
- Kidney stones can cause sharp pain in the lower back, usually on one side
- Endometriosis (the buildup of uterine tissue in places outside the uterus)
- Fibromyalgia (a chronic pain syndrome involving widespread muscle pain and fatigue)
- Tumors that press on or destroy the bony spine or spinal cord and nerves or outside the spine elsewhere in the back
- Pregnancy (back symptoms almost always completely go away after giving birth)
A detailed discussion about spine pain can take forever. Consult our team. we will give you the time and attention you Deserve to diagnose your case and formulate a treatment plan. text your name and phone number to 833-547-7463 (833-LI-SPINE).
References:
[7] Courtesy: Radiology Masterclass
[8] Figures from Corbett S. Introduction to Spine Surgery. 1st ed. Stuttgart New York: Georg Thieme Verlag; 2006.