Nimbus RFA Radiofrequency Ablation
Introduction
Neuro-destructive procedures have been used to treat medical conditions for over a century. Nerves carry pain signals and targeted destruction of nerve tissue can achieve reduction or elimination of pain signals reaching the brain. Historically, alcohol or phenol was used as agents to destroy nerve cells. Injection of these agents is uncontrolled and unpredictable, even when small volumes are used. Radiofrequency neurotomy or ablation (RFN or RFA) was invented to destroy nerve tissue in a more controlled manner. Radiofrequency currents generate heat. These currents, when delivered through a needle, can create precise thermal lesions leading to tissue destruction. Skillfully created targeted lesions can selectively destroy nerves responsible for transmitting and/or modulating the signals of pain.
RFA is an established treatment which continues to evolve since its invention in the early 1970s. The treatment was initially used to treat back and neck pain originating from facet joints. Over the last decade, its use has expanded to treat several other pain syndromes, including chronic joint pain conditions affecting sacroiliac joints, shoulders, hips, and knees. I will spend a few minutes explaining the differences in various RF options.
Types of Radiofrequency Ablations:
Conventional Continuous Radiofrequency (CRF) – CRF uses high-frequency alternating current to induce coagulative necrosis in the target tissue. Tissue destruction occurs at probe temperatures between 60° and 80° C. With CRF, the magnitude of tissue destruction is related to the temperature of the tissue, the size of the electrode as well as the duration of the procedure.
Not in the distant past, we were making lesions using a thin 22-gauge insulated needle with an active tip to create lesions near sites where medial branches are “supposed to” run. The procedure is done under fluoroscopic guidance. X-ray guidance can only help to guide positioning of the needle tip at the desired location. We cannot see these nerve branches. Depending on doctors’ preference, 1-3 lesions are created at each site to “capture” as many nerve branches as feasible. Higher numbers of lesions lead to better and longer lasting results.
Pulsed radiofrequency (PRF): PRF was introduced in 1998. PRF uses streams of radiofrequency current in short high-voltage bursts (20 ms) followed by the “silent” phase (480 ms) which allows time for heat elimination, generally keeping the target tissue below 42°C. Histopathologic work has shown that PRF at 42°C causes only transient endoneurial edema, while destructive wallerian degeneration is seen with CRF at 80°C. Since thermal damage from PRF is minimal and not how PRF exerts its clinical effect, it can be used at mixed sensory and motor nerves (like sciatic nerve), and even dorsal root ganglion. We are successfully using this technique to treat chronic radicular pain, ilioinguinal, genitofemoral and intercostal neuralgia.
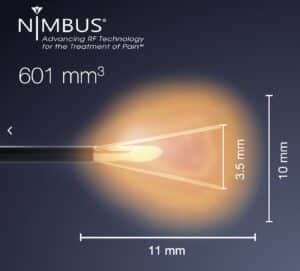
- Large Volume Radiofrequency (LVRF): As the understanding of better results with larger lesions grew, there was a growing demand for needles that could create bigger legions. Coolief, Venom, Trident, SideKick and, more recently, Nimbus needles have been introduced to achieve this goal. Of all these names, the Nimbus needle creates the biggest lesion in the shortest amount of time. We recently introduced the Nimbus cannula to Long Island for the very first-time.
- Water-Cooled Radiofrequency (WCRF): Water-Cooled radiofrequency ablation method (Coolief) also uses targeted heat lesions, but the needle tip is “cooled” to slightly lower temperatures (60°C, instead of 80°C) with constant flow of water. The slightly lower temperatures achieved with this system allowed for larger lesions to be performed without inducing tissue charring. Unfortunately, most clinicians report equipment problems complicating the treatment. The procedure takes longer, and equipment troubles are not uncommon during multi-lesion technique.
- Nimbus: The Nimbus needle was developed in 2009 by a Denver pain specialist, Dr. Robert Wright, who used his wife’s four-prong gem tweezers to create the first tined needle concept. The lesion created by his experimental device was consistently globular or cloud-shaped, hence the name, “Nimbus”. In contrast to Coolief, Nimbus RF technique is far less cumbersome. The Nimbus needle creates the largest volume of targeted lesion of all available options on the market. Our early results from using this needle and system have been nothing but spectacular. At present, we are the only group on Long Island using this device.
 |
 |
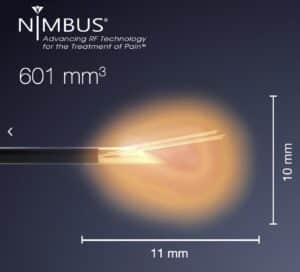 |
| Nimbus Needle with deploable tines and the large size lesion it creates. Courtesy: Stratus Medical |
||
Conclusion
Radiofrequency ablation remains one of the bedrock foundational techniques of interventional pain medicine. We have been using this procedure to successfully treat neck, mid-back and lower back pain related to facet syndrome for decades. Refinements of this technique have extended its use to treat chronic pain syndromes related to joint pain (sacroiliac, shoulder, hip, knee) and many neuropathic pain conditions. We have proudly introduced the latest advancements of RFA on Long Island as a testament of our quest for perfection.
Amit Sharma MD
Director of Interventional Spine, SpinePain Solutions
Chief, Division of Pain, Good Samaritan University Hospital
Medical Director, Minimally Invasive Center of New York