Radiofrequency Neuroablation or Rhizotomy
Welcome to our information page about radiofrequency ablation (RFA), neurotomy, or rhizotomy. This article will focus on the basics of this technique and the painful conditions it can be used to treat.
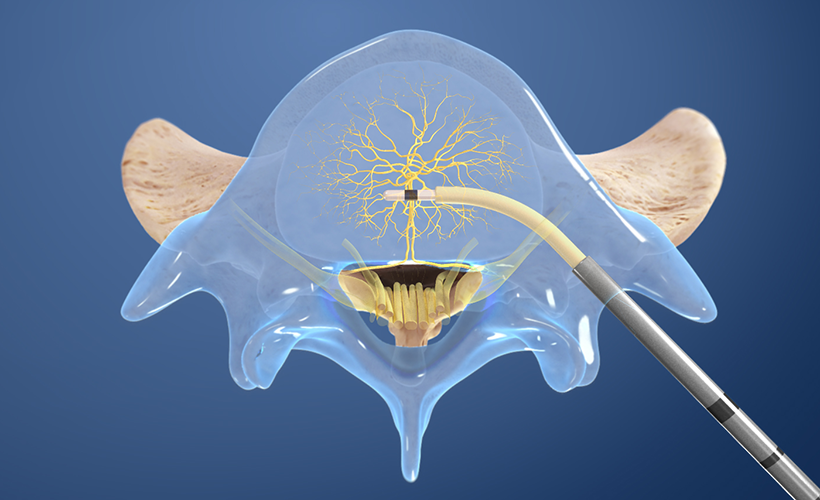
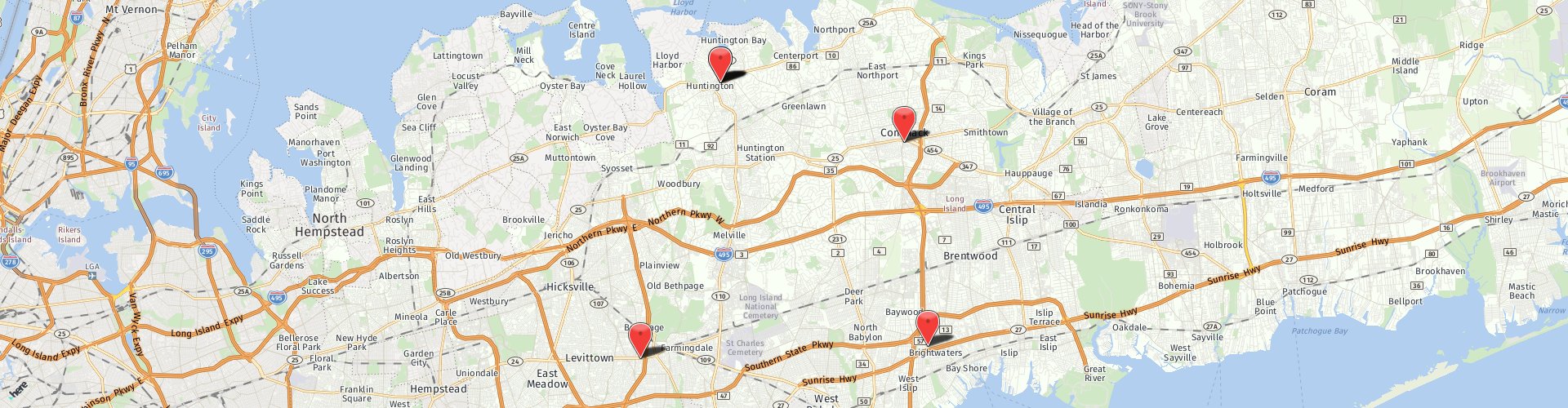
Dr. Sharma is one of the few physicians on Long Island who is currently offering all types of RFA options; from conventional continuous high heat RFA (for neck, mid-back and low back pain) using most advanced techniques (NIMBUS), water-cooled moderate temperature RFA (Coolief for shoulder, hip, knee, sacroiliac joint related pain, intracept for vertebrogenic low back pain), low temperature RFA for delicate structures (pulsed RFA for chronic radiculopathy), to cryoablation (occipital neuralgia) and chemical neurolysis (intercostal nerves for chest pain related to shingles). He also performs neurotomy for several painful nerve condition like occipital headaches, neuralgia paresthetica, intercostal neuralgia and chemoablation for cancer related pain. He is the only physician on Long Island currently offering the most advanced option of pulsed radiofrequency ablation of dorsal root ganglion for patients who cannot (or do not want to) undergo decompressive back surgery for “pinched nerve related sciatica”. He is also performing advanced radiofrequency techniques like intracept (basivertebral nerve ablation).
Understand Basic Neuroanatomy
Your brain works as a supercomputer. To run your body efficiently, it sends and receives signals from most organs and tissues (skin, muscles) through small neuronal-wires, which are called “nerves” in medical terms. A short lesson on the basics of human neuroanatomy is important to understand this topic fully.
Brain (housed inside your skull) and spinal cord (protected within your back bone or spinal column) together are considered central nervous system. Destruction to any part of the central nervous system could be devastating. Stroke or spinal cord injuries are examples of conditions where injury to central nervous tissue occur. The central nervous system communicates with the rest of the body and the outside world with three different types of nerves (peripheral nervous system):
- Cranial Nerves: These nerves carry important signals of smell, sound, taste and vision directly to the brain.
- Autonomic Nerves: These nerves help control heart rate, breathing, digestion, urination etc.
- Spinal Nerves: Based on the specific signals they carry, spinal nerves can be
- Sensory Nerves (carrying signals of pain/touch/temperature/pain to the spinal cord),
- Motor Nerves (carrying signals from the spinal cord to the muscles) and
- Mixed Nerves (containing both varieties).
Now that you know the basic framework of your nervous system, let’s focus on one of the most important signal it communicates: PAIN.
The Concept Behind Neuronal Destruction
Pain is a sensory and an emotional experience. Past experiences of pain help you avoid injuries. When you do get injured, pain helps you avoid further damage to the involved area. In some conditions, pain becomes a nuisance and needs to be blocked. Pain can be blocked, or reduced, by:
- Curing the underlying condition
- Suppressing central nervous system (brain and spinal cord) from receiving painful signals (using drugs), or
- Destroying the nerves that carry painful signal to the spinal cord (and brain)
In a perfect world, the only part of central or peripheral nervous system that we ever want to destroy are the small nerves that carry pain signals to the brain. The idea of destroying pain carrying nerves has always fascinated scientists and doctors. It can be achieved using a chemical agents (neurolysis), freezing cold temperatures (cryoablation) or heat (radiofrequency ablation or rhizotomy).
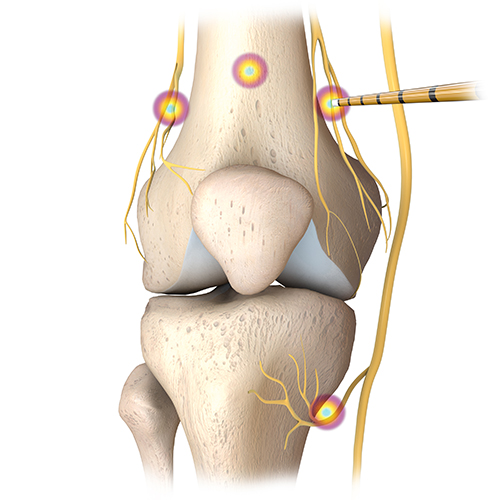
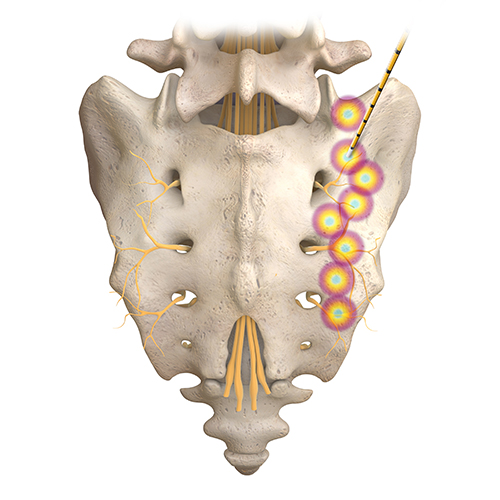
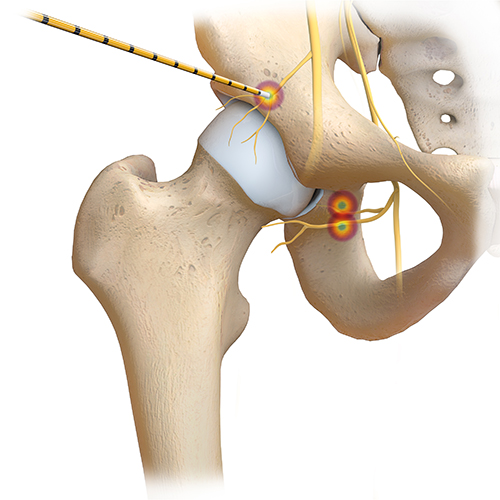
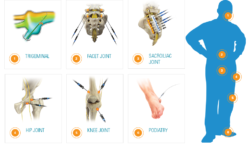 Radiofrequency ablation has been used to destroy pain carrying nerve endings for many medical conditions. In pain management world, it has historically been used to deaden the pain carrying nerve endings of spinal facet joints (medical branches). Recently this technology has been sophisticated to destroy pain carrying nerve fibers of:
Radiofrequency ablation has been used to destroy pain carrying nerve endings for many medical conditions. In pain management world, it has historically been used to deaden the pain carrying nerve endings of spinal facet joints (medical branches). Recently this technology has been sophisticated to destroy pain carrying nerve fibers of:
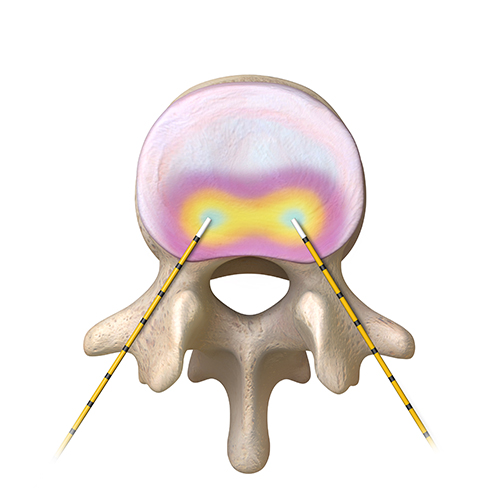
- Vertebral bone (Intarcept)
- Degenerated disc (IDET, Transdiscal Coolief)
- Sacroiliac joint (L5 dorsal ramus and sacral lateral branches)
- Hip (articular branches of the obturator and femoral nerves) and
- Knee joint (genicular nerves)
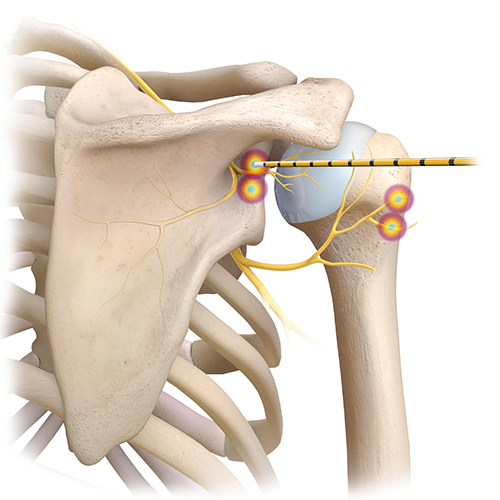
- Shoulder joint (articular branches of the axillary, suprascapular and subscapular nerves)
The remainder of this article will focus on facet joint radiofrequency ablation. Please also consider exploring our website to learn more about facet arthropathy (facet syndrome) and medial branch block (an interventional technique to diagnose pain related to facet joint arthritis).
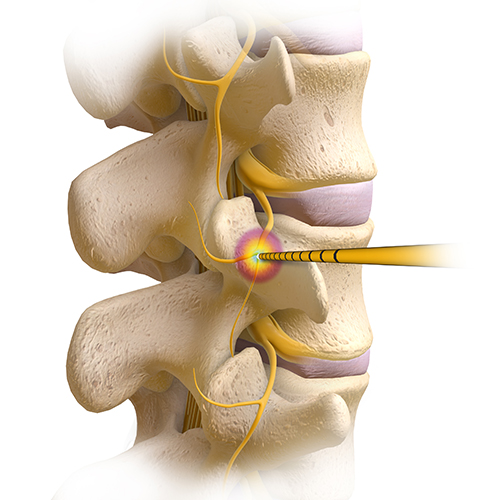
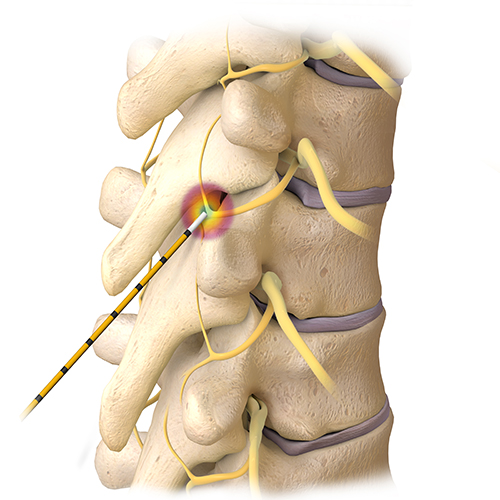
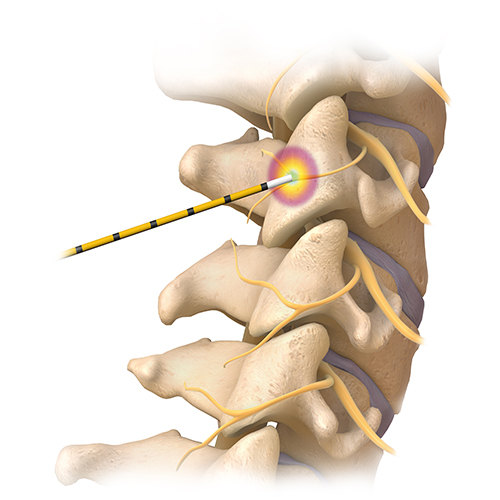
Radiofrequency rhizotomy, also known as neurotomy, is a minimally invasive procedure for treating nerve pain in the spine. The procedure works by sending pulses of heat energy generated by radio-waves to the affected nerves. The goal is to stop these nerves from processing pain signals from injured facet joints, the small joints located between the vertebrae.
Normally this method of pain management is not used unless the patient’s pain has not responded to other more conservative treatments, such as anti-inflammatory medication or physical therapy. The goal of a radiofrequency rhizotomy is to reduce back pain without reducing nerve function. Diagnostic testing is usually performed before the procedure to make sure precisely which nerves are causing the problem.
The Procedure
During a radiofrequency rhizotomy, the patient lies face down. The procedure is outpatient, performed under local anesthesia with intravenous sedation. It takes approximately 20-30 minutes. After numbing the site, the surgeon uses a small needle to penetrate the skin covering the spine. The highly focused heat targets the affected nerve(s), preventing pain signals from being transmitted to the brain.
Fluoroscopy, an imaging technique, is used during the process to ensure that the small needle is inserted accurately over the appropriate facet. Depending on the patient’s condition, the needle may be inserted into more than one place on the spine.
The technical aspects of each RFA technique are beyond the scope of this article. Consider discussing this topic further with your pain doctor. There are few important issues to mention. The effectiveness of rhizotomy procedure depends on choosing the right candidate for the procedure. It is equally important that your doctor is an expert at making small, targeted lesions to destroy pain carrying nerve endings, while saving the vital nerves that send signals of sensation or strength to your arms and legs.
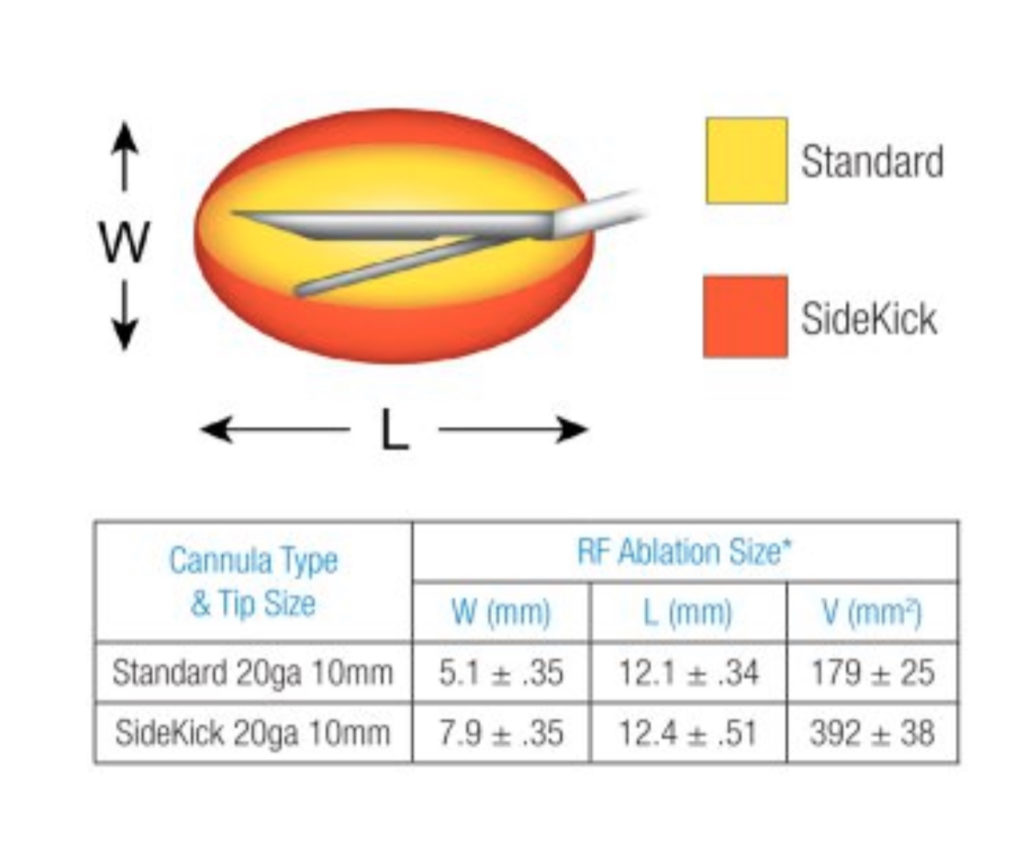
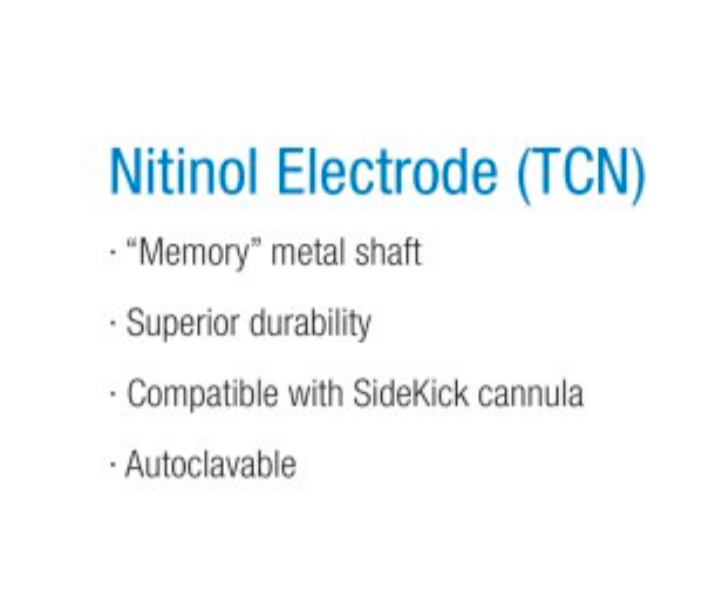
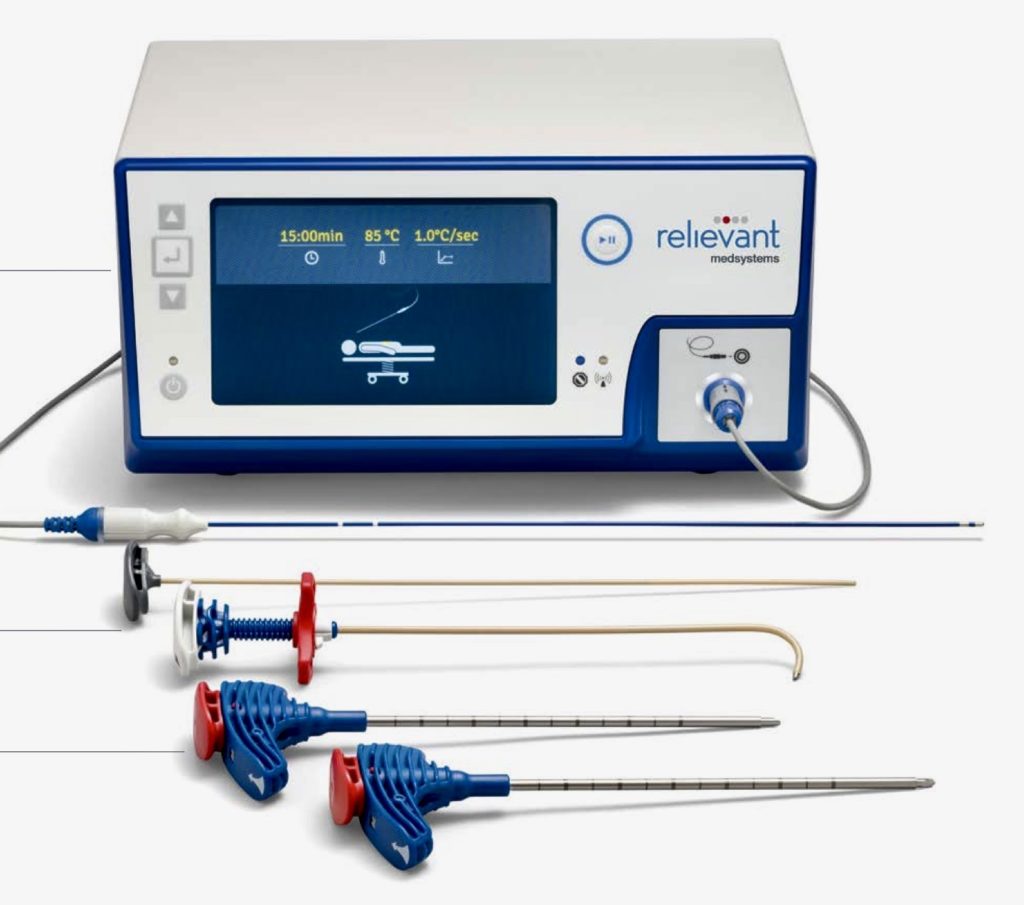
Although your doctors training and experience are important, the equipment they use also play a role in the procedural success. As an example, the size of lesion created by RFA needles varies from needle types. Under Dr. Sharma’s supervision, Good Samaritan University Hospital Pain Center has acquired the most advanced systems currently available in the market. We only utilize Cosman G4 and Avanos Coolief generators. We depend on the state of the art nitinol memory introducers along with Nimbus and SideKick RF cannulas for exceptional RF lesions creation, while maintaining the highest industry safety standards.
After The Radiofrequency Rhizotomy
Patients should be able to resume normal activities the day after the procedure, although they may expect some soreness, numbness, itchiness or weakness in the targeted region for a few weeks. After about 3 weeks, they should be pain-free. As with most pain management treatments, radiofrequency rhizotomy does not work equally well for all patients. While symptom relief from the neurotomy is always temporary, it may provide comfort for several months or for more than a year.
Risks Of Radiofrequency Rhizotomy
While the procedure is generally considered a safe one, because nerves are affected there is some element of risk. Although extremely rare, serious complications are possible, including long-term numbness, worsening of pain or weakness.