Coccyx Tailbone Injection
The coccyx is the terminal segment of the spine that consists of 3 to 5 fused bone segments. It attaches to sacrum with sacrococcygeal ligament. Coccyx has several important functions. It acts as the insertion site for multiple muscles, ligaments, and tendons, which help support the pelvic floor and also contribute voluntary bowel control. Coccyx also serves as one leg of the tripod, and along with the ischial tuberosities, provides weight-bearing support to a person in the seated position. Coccyx also provides positional support to the anus.
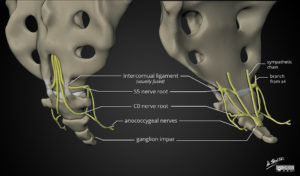
Coccygeal Plexus
Coccyx receives nerve supply from a network of nerves, the coccygeal plexus (Courtesy of Dr Matt Skalski, Radiopaedia.org. From the case rID: 63690). Blocking coccygeal nerves or coccygeal plexus has been shown to help with coccydynia or tailbone pain.
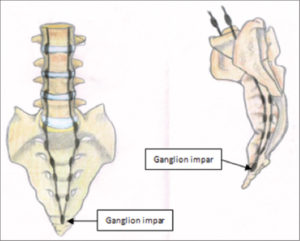
Ganglion of Impar (Courtesy: Asian Journal of Neurosurgery)
In addition, the pelvic portion of each sympathetic trunks converge and end on the front of the coccyx in a small ganglion, the ganglion impar, also known as azygos or ganglion of Walther. There is a strong evidence that this bundle of nerves also carries pain signals in cases of coccydynia. Blocking coccygeal nerves (or coccygeal plexus) along with the ganglion of impar, has been shown to help with coccydynia or tailbone pain. Imaging guidance, such as fluoroscopy, is absolutely recommended for injections around the coccyx because of its position relative to other vital structures.
Coccydynia
Coccydynia, or coccygodynia, is pain in the region of the coccyx or tailbone. Treatment of tailbone or coccygeal pain can be difficult and sometimes controversial because of the multifactorial nature of coccygeal pain. Many physiologic and psychological factors contribute to its cause. Most cases of coccydynia resolve within weeks to months with or without conservative treatment, but for a few patients, the pain can become chronic and debilitating.
Obesity and female gender are often cited as predisposing factors to develop tailbone pain. Women are 5 times more likely to develop coccydynia than men. Presumably, rapid weight loss can also be a risk factor because of the loss of mechanical cushioning. The most common cause of coccydynia is external or internal trauma. External trauma usually occurs due to a backwards fall, leading to a bruised, dislocated, or broken coccyx. The location of the coccyx makes it particularly susceptible to internal injury during childbirth, especially during a difficult or instrumented delivery. Minor trauma can also occur from repetitive or prolonged sitting on hard, narrow, or uncomfortable surfaces. Nontraumatic coccydynia can result from hypermobility or hypomobility of the sacrococcygeal joint.
Conservative treatment is successful in 90% of coccydynia cases. Relatively simple measures like a modified wedge-shaped cushions (coccygeal cushions) or circular cushions (donut cushions) have been suggested for the treatment of coccydynia. Coccygeal cushions can relieve the pressure on the coccyx while the patient is seated. Donut cushions can place pressure on the coccyx by isolating the coccyx and ischial tuberosities and are more useful for treating rectal pain. Postural training, heat and cold applications and antiinflammatory medications are helpful in many cases.

For the few cases that do not respond to these conservative treatments, more aggressive treatments may be indicated. Pelvic floor rehabilitation can be helpful for coccydynia that is associated with pelvic floor muscle spasms. Manual manipulation and massage can be both diagnostic and therapeutic. Intrarectal manipulation can identify and potentially correct a dislocated sacrococcygeal joint. Manual manipulation and massage can help relieve associated muscle spasms or ligament pain.
In a handful of cases, a combination of coccygeal nerve block and ganglion of impar block has been shown to an extremely successful treatment option to resolve pain. Surgical resection of coccyx (coccygectomy) is rarely needed.
Procedure
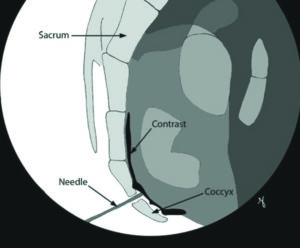
Ganglion of Impar Injection (Courtesy: Ainsworth Institute)
You may be given a laxative the night before procedure to keep your rectum “empty”. After admission process is completed, you will be taken to the procedure suite. You will be positioned in a comfortable position and anesthesia is induced by an attending anesthesiologist. Fluoroscopic images (X-Ray) is used to identify the site of needle entry. A thin Cannula (needle) is placed under live fluoroscopic guidance to the target sacrococcygeal opening and various safety steps are conducted to confirm accurate location. Injection of planned medication is made and needle are withdrawn out of sacrococcygeal space. Needle is then redirected to block sacrococcgeal nerves. Needle is finally withdrawn. A band-aid is applied at the needle entry site and patient is taken to recovery area.
In selective cases, regenerative medicine options like platelet rich plasma treatment may be offered. Platelet-rich-plasma (PRP) injections use components of the body’s own blood to stimulate healing. Platelets, which are usually associated with coagulation (clotting), may assist in mending and strengthening damaged tissue by increasing certain growth factors. During the normal healing process, the body uses platelets to promote new-tissue growth and repair injuries. By supplementing platelet content, the healing process is accelerated. There is ongoing research on the efficacy of PRP injections, and some medical professionals remain skeptical about their value.
Last, but not the least, DRG stimulation has shown some positive results in treatment of coccydynia and it might be worth a trial before you ever consider coccygectomy.
Risks and complications
- Bleeding or bruising at the needle insertion site
- Infection
- Nerve Injury
- Aggravation of pain
References:
- Buttaci CJ, Foye PM, Stitik TP: Coccydynia successfully treated with ganglion impar blocks: A case series. Am J Phys Med Rehabil 2005;84:218.
- Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner J. 2014;14(1):84-87.
- Mostafa E, Varacallo M. Anatomy, Back, Coccygeal Vertebrae. [Updated 2020 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549870/