Pain Management in Huntington
So, your doctor has referred you to pain management In Huntington.
You may have reservations about this step. Why would you want to “manage” your symptom (pain) when common sense would suggest to find the real problem and fix it? You may have been hearing horrible news stories in media about the drug epidemic our nation is facing. Wouldn’t seeing a pain management specialist in Huntington mean getting on addictive medications?

Pain management is a vast and evolving field. “Interventional” Pain Management doctors are specialists in dealing with spine and major joint problems. During their training, pain physicians go through rotations in neurology, physician medicine rehabilitation, radiology, oncology, orthopedics and neurosurgery. Depending on their training and background, they may focus on spine or joint problems or both with their clinical practice. Pain Management doctors help to reduce acute inflammation affecting a particular area of spine through minor injections. This step helps your chiropractor or physical therapist work on your neck or back more efficiently.

At times, your primary doctor might refer you to pain management in Huntington to address your sciatica or acute pain condition through a spine injection when it is expected to heal on its own eventually. In some conditions, they are able to fix the underlying problem (like a cement injection for spinal fracture) or radiofrequency ablation of a painful arthritic spinal joint. Occasionally they do offer a short course of oral medications to help your pain while your condition resolves. The good news is that most patients who are referred to pain specialists only see them for few weeks to months.
 Let us start the journey of educating you about your condition and ways to control the pain related to it, or better heal it altogether!
Let us start the journey of educating you about your condition and ways to control the pain related to it, or better heal it altogether!
We suggest you start with learning a bit about your back pain. For many other conditions, you can review our resources section from the drop-down menu or visit our “video library“.
If you are one of our trusted referring provider, you can download our patient brochure here.
Interventional Spine Surgery and Pain Management In Huntington
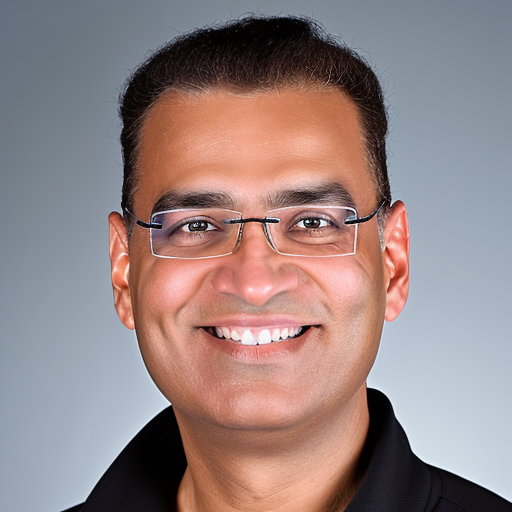
Amit Sharma MD
- Board Certified in Interventional Spine Surgery & Pain Management
- Castle Connolly Regional Top Doctor: 2016-2023
- Top Doctors New York Metro Area: 2016-2023
-
New York Magazine Top Doctors: 2017-2023
-
Newsday Top Doctors on Long Island: 2016-2023
-
Completed residency from Columbia University in New York City and fellowship training in Interventional Pain from Johns Hopkins University
- Assistant professor at Columbia University (2007-09)
- Founder of SpinePain Solutions
- Chief, Division of Pain Management at Good Samaritan Hospital Medical Center
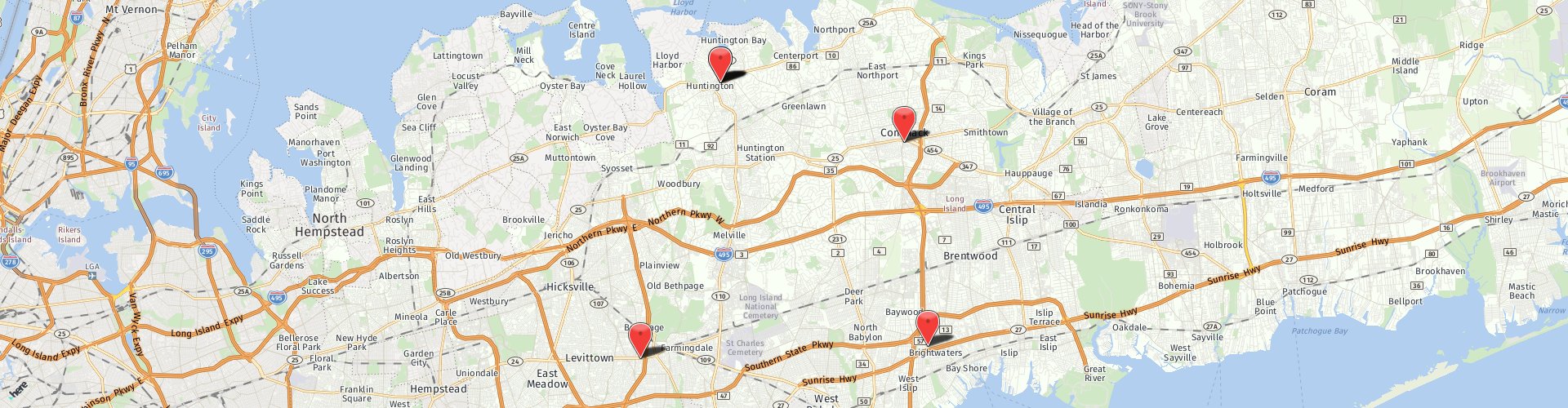
Dr. Amit Sharma is a board certified physician who specializes in interventional pain management in Huntington, NY. He is the Chief of the Division of Pain Management at Good Samaritan University Hospital. He is the founder and Director of Interventional Spine & Pain at SpinePain Solutions and Medical Director at Minimally Invasive Center of New York.
Recognized by his peers for his skills, commitment, and an outstanding professional path; Dr. Sharma has been honored by Castle Connolly, New York Magazine and Newsday as one of the Top Doctors in the US for Pain Management for the last several years. He has simultaneously received “Patients Choice Awards” and “Compassionate Doctor Award” for many years. He is a lifetime member of American Society of Interventional Pain Physicians and a member of numerous national and international pain societies.
Dr. Sharma did his residency in anesthesiology at The College of Physicians & Surgeons of Columbia University in New York City. On completion, he was rewarded as the best resident of the year. He then obtained fellowship training in interventional pain medicine at Johns Hopkins School of Medicine. He was honored with Pfizer best fellow of the year by Johns Hopkins. Dr. Sharma served as an Assistant Professor at Columbia University prior to going in private practice.
Having performed over 25,000 interventional procedures, Dr. Sharma specializes in the diagnosis and management of back and neck problems, along with neuropathic and cancer pain. He also has special interest in ischemic pain and peripheral vascular disease related issues. He has an expertise in neuromodulation (spinal cord stimulation), intrathecal drug delivery systems, minimally invasive spine procedures (Kyphoplasty, Intradiscal Electrothermy, Nucleoplasty, MILD, Intracept, Endoscopic Discectomy and Rhizotomy) and radiofrequency ablative procedures. Along with the other physicians at SpineCare Long Island, he is a strong proponent of non-operative options such as physical therapy, chiropractic manipulations and acupuncture.
Dr. Sharma is well published in peer-reviewed journals and has authored numerous textbook chapters. He has been invited as a guest speaker at several national pain meetings. He has also done research in the field of Complex Regional Pain Syndrome (CRPS or RSD). His team at Johns Hopkins was provided a financial grant to conduct the largest study on CRPS patients which was published in a renowned journal. Having served as a teaching faculty, training residents and fellow doctors, Dr. Sharma carries the passion of education with him. He believes in educating patients and spends time explaining every aspect of their treatment plan with them.
Publications (In Peer Review Literature)
- Gharibo C, Sharma A, Soin A, Shah S, Diwan S, Buenaventura R, Nampiaparampil DE, Aydin S, Bakshi S, Abdi S, Jha SS, Cordner H, Kaye AD, Abd-Elsayed A, Candido KD, Knezevic NN, Atluri S, Wargo BW, Sanapati MR, Datta S, Hirsch JA, Manchikanti L, Rajput K. Triaging Interventional Pain Procedures During COVID-19 or Related Elective Surgery Restrictions: Evidence-Informed Guidance from the American Society of Interventional Pain Physicians (ASIPP). Pain Physician. 2020 Aug;23(4S):S183-204. PMID: 32942785.
- Sharma A, Agarwal S, Broatch JW, Raja SN. A Web Based Epidemiological Survey of Complex Regional Pain Syndrome. Reg Anesth Pain Med. 2009 Mar-Apr; 34(2):110-5.
- Sharma A, Williams K, Raja SN. Advances in treatment of complex regional pain syndrome: recent insights on a perplexing disease. Curr Opin Anaesthesiol. 2006 Oct;19(5):566-572.
- Sharma A, Pagel PS, Bhatia A. Intraoperative iatrogenic acute pericardial tamponade: use of rescue transesophageal echocardiography in a patient undergoing orthotopic liver transplantation. J Cardiothorac Vasc Anesth. 2005 Jun;19(3):364-6.
- Jooste EH, Sharma A, Zhang Y, Emala CW. Rapacuronium Augments Acetylcholineinduced Bronchoconstriction via Positive Allosteric Interactions at the M3 Muscarinic Receptor. Anesthesiology. 2005 Dec;103(6):1195-1203.
- Christo PJ, Hobelman JG, Sharma A. Aging and the Neurobiology of Addiction. J Geriatrics & Aging, 2005 Nov/Dec;8(10):48-52.
Editorial Experience
- Section Editor (Acute and Chronic Pain): Marcucci: Avoiding Common Anesthesia Errors, Catherine Marcucci, Norman A. Cohen, David G. Metro, Jeffery R. Kirsch (Eds), Lippincott Williams & Wilkins, 2008.
- Referee, Cochrane Pain, Palliative & Supportive Care (PaPaS) Review Group (2007 – Present).
Textbook Chapters
- Sharma A, Raja SN. Assessment and Management of Chronic Pain and Palliative Care. In: Geriatric Anesthesia, Fredirick E. Sieber (Ed.). The McGraw-Hill Companies, Inc., 2007. PP 319-336.
- Sharma A. The basal infusion mode in patient controlled analgesia is both friend and foe, In: Marcucci: Avoiding Common Anesthesia Errors, Catherine Marcucci, Norman A. Cohen, David G. Metro, Jeffery R. Kirsch (Eds), Lippincott Williams & Wilkins, 2008. PP 725-30.
- Sharma A. Rule out facet arthropathy before initiating expensive and invasive maneuvers for back and spine pain, In: Marcucci: Avoiding Common Anesthesia Errors, Catherine Marcucci, Norman A. Cohen, David G. Metro, Jeffery R. Kirsch (Eds), Lippincott Williams & Wilkins, 2008. PP 741-47.
- Sharma A. Do not guess at the equivalent dose when determining an opioid conversion, In: Marcucci: Avoiding Common Anesthesia Errors, Catherine Marcucci, Norman A. Cohen, David G. Metro, Jeffery R. Kirsch (Eds), Lippincott Williams & Wilkins, 2008. PP 712-19.
- Sharma A. Management of perioperative pain in opioid dependent patient – Out of the frying pan, into the fire, In: Marcucci: Avoiding Common Anesthesia Errors, Catherine Marcucci, Norman A. Cohen, David G. Metro, Jeffery R. Kirsch (Eds), Lippincott Williams & Wilkins, 2008. PP 732-35.
- Sharma A., Kathuria SS. Anesthesia for eye surgery – The innate culture of “1-N-1”, In: Marcucci: Avoiding Common Anesthesia Errors, Catherine Marcucci, Norman A. Cohen, David G. Metro, Jeffery R. Kirsch (Eds), Lippincott Williams & Wilkins, 2008. PP 339-343.
- Sharma A. Consider the paramedian approach for the thoracic epidural placement, especially at the mid-thoracic level, In: Marcucci: Avoiding Common Anesthesia Errors, Catherine Marcucci, Norman A. Cohen, David G. Metro, Jeffery R. Kirsch (Eds), Lippincott Williams & Wilkins, 2008. PP 441-46.
- Sharma A. Consider discussing use of ketorolac (toradol) in perioperative setting with your surgical team before the need arises, In: Marcucci: Avoiding Common Anesthesia Errors, Catherine Marcucci, Norman A. Cohen, David G. Metro, Jeffery R. Kirsch (Eds), Lippincott Williams & Wilkins, 2008. PP 720-24.
- Sharma A., Campbell JN, Raja SN. Sympathetic Blocks for Pain, In: The Senses: A Comprehensive Reference, Volume 5, Allan I. Basbaum, Peter Dallos, Gary K. Beauchamp, Jon H. Kaas, M. Catherine Bushnell (Eds), Elsevier Company, 2007.
- Sharma A., Raja SN. Chronic Pain and the Sympathetic Nervous System: Mechanisms and potential implications for pain therapies, In: Translational Pain Research. Volume 2: Comparing Preclinical Studies and Clinical Pain Management.
- Lost in Translation?, Jianren Mao (Ed), Nova Science Publishers, Inc., 2006. PP 169- 188.
- Sharma A., Raja SN. CRPS: Current Diagnosis and Therapy. Wilson PR, Stanton- Hicks M, Harden RN (Eds) Progress in Pain Management Research, Vol 32. IASP Press, 2005; Book Review. Clin J Pain. 2006 Feb;22(2):225.
Electronic Publications
- Sharma A., Raja SN. Use and abuse of opioids: The eternal debate. Original Article.
- MD Consult: Pain Medicine, Perspectives on contemporary topics. Retrieved on Feb 7, 2005 from www.mdconsult.com
- Sharma A., Raja SN. Sex differences in clinical pain: The need for further research.
- Editorial. MD Consult: Pain Medicine, Perspectives on contemporary topics. Retrieved on Jan 5, 2005 from www.mdconsult.com
CLICK HERE TO SCHEDULE AN APPOINTMENT WITH DR. SHARMA
What are the 3 different types of pain management in Huntington?
The three main types of pain management in Huntington are:
- Medication-based approaches: This includes over-the-counter medications like acetaminophen or ibuprofen, prescription medications such as opioids, antidepressants, and anticonvulsants, and topical treatments like creams or patches.
- Non-medication-based approaches: These methods focus on techniques and therapies that don’t involve medication. Examples include physical therapy, occupational therapy, massage therapy, acupuncture, chiropractic care, cognitive-behavioral therapy (CBT), relaxation techniques, and biofeedback.
- Interventional procedures: These procedures are more invasive and are typically performed by specialists. They include nerve blocks, injections (such as epidural injections or joint injections), radiofrequency ablation, spinal cord stimulation, and surgeries like decompression surgeries or implantation of pain-relief devices.
What to do when chronic pain is unbearable?
When chronic pain becomes unbearable, it’s essential to take proactive steps to manage it effectively. Here are some strategies you can consider:
- Consult a Healthcare Professional: Schedule an appointment with a doctor such as a pain management specialist. They can assess your condition, review your pain management plan, and recommend adjustments or additional treatments.
- Medication Adjustment: Your healthcare provider may adjust your current medications or prescribe new ones to manage your pain better. This could include more potent pain relievers, muscle relaxants, anti-inflammatory drugs, or medications that target nerve pain.
- Physical Therapy: They specialize in pain management. PT’s can craft a a program to help improve flexibility, strength, and mobility, which can help alleviate pain and prevent further complications.
- Mind-Body Techniques: Explore mind-body techniques such as relaxation exercises, deep breathing, meditation, mindfulness, yoga, tai chi, or biofeedback. These practices can help reduce stress, improve coping skills, and lessen pain perception.
- Complementary Therapies: Consider complementary therapies like acupuncture, massage therapy, chiropractic care, or aromatherapy. These treatments may provide additional relief and promote overall well-being.
- Psychological Support: Chronic pain can impact your mental health. Seek support from a psychologist, counselor, or support group specializing in chronic pain management. Cognitive-behavioral therapy (CBT) can address the emotional aspects of pain and developing coping strategies.
- Lifestyle Modifications: Make lifestyle changes that can support pain management, such as maintaining a healthy diet, exercising regularly within your limits, practicing good sleep hygiene, managing stress effectively, and avoiding activities that worsen your pain.
- Explore Interventional Procedures: If conservative treatments are insufficient, your doctor may recommend interventional procedures such as nerve blocks, epidural injections, radiofrequency ablation, or spinal cord stimulation. These procedures target specific areas of pain and can provide significant relief for some individuals.
- Stay Informed: Educate yourself about your condition, treatment options, and self-management strategies. Being informed allows you to make decisions about your health and advocate for the best care possible.
- Seek Support: Lean on friends, family, and support networks for emotional and practical assistance. Chronic pain can be challenging to manage alone, and having a solid support system can make a difference in your overall well-being.
Remember that managing chronic pain often requires a multifaceted approach tailored to your individual needs. It may involve a combination of treatments, lifestyle adjustments, and ongoing support to achieve the best outcomes.
What pain level is considered severe?
 Pain intensity is subjective and can vary significantly from person to person. However, healthcare professionals often use a pain scale to assess and categorize pain levels. One of the commonly used pain scales is the numerical rating scale (NRS), which ranges from 0 to 10:
Pain intensity is subjective and can vary significantly from person to person. However, healthcare professionals often use a pain scale to assess and categorize pain levels. One of the commonly used pain scales is the numerical rating scale (NRS), which ranges from 0 to 10:
- 0: No pain
- 1-3: Mild pain (annoying but does not interfere significantly with daily activities)
- 4-6: Moderate pain (interferes with daily activities but can still be managed)
- 7-9: Severe pain (substantially interferes with daily activities and may require immediate attention)
- 10: Worst possible pain
Therefore, pain levels rated between 7 and 10 on the NRS are generally considered severe. However, it’s crucial to understand that pain perception is unique to each individual and can be influenced by various factors, including individual pain thresholds, emotional state, and the nature of the pain (e.g., acute vs. chronic). Healthcare providers, recognizing this individuality, may also consider other factors such as the impact of pain on functioning and quality of life when determining the severity of pain and planning appropriate management strategies.
If you’re interested in pursuing pain management in Huntington, you should consider the services of Dr. Sharma and his team. Please click here to schedule an appointment.